ASD Device Closure
Atrial septal defect
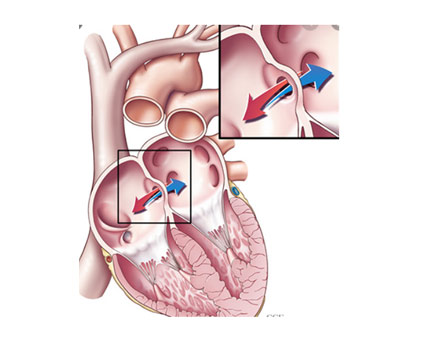
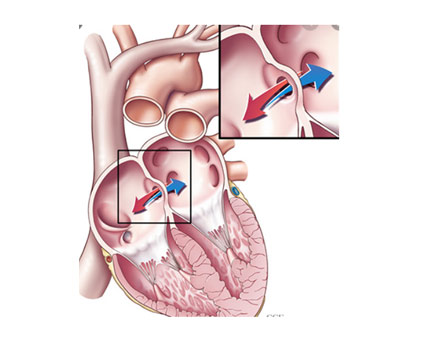
- An atrial septal defect is an opening in the atrial septum – the wall dividing the two upper chambers of the heart
- It is a congenital defect

Atrial septal defect
- An atrial septal defect allows oxygen rich blood to pass from the left atrium across the atrial septal opening and mix with oxygen poor blood in the right atrium.
Problems with ASD
- Right heart dilatation
- Right heart failure
- High blood pressure in lungs – pulmonary hypertension
- Frequent chest infections
- Heart rhythm problems
ASD closure Problems with ASD
Trans-catheter ASD closure
- 20 year follow up results are comparable to surgical closure

ASD – When to Intervene
| Type | TIMING | INTERVENTION |
|---|---|---|
| Secundum ASD Asymptomatic | >3 years/ > 10 KG | Device closure (80%) Surgery |
| Symptomatic | Any age > 1 year | Surgery > device |
| Primum ASD | 1- 2 years | Surgery |
| SV ASD | >2 years | Surgery |
Steps in ASD Closure
- Local anesthesia in adults, Short GA in children
- Prepare the groin
- Femoral vein access
- catheter – wire – enter Pulmonary artery – check pressures
- Same catheter combination – cross the defect into the pulmonary vein (across the ASD)
ASD steps
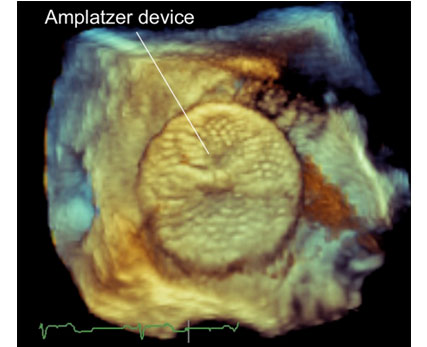
- Catheter in PV – exchange with a extra stiff wire –
- With stiff wire in place – take the appropriate sheath into the Left Upper PV
- The loaded device is taken across in the sheath
- The device is deployed across the defect
- Position is confirmed on ECHO before release
ASD Device
Situations where device closure not suitable
- Primum ASD
- Sinus Venosus ASD
- Large secundum ASD( >35mm) with absent margins(especially infero-posterior)
- Large II ASD in small children (< 3 years/ < 10Kg)
Difficult ASD closure -Deployment
To have the RA disc aligned to the septum on the RA side before the LA disc can slip out
- Rapid deployment
- Right upper pulmonary vein
- Partly trapping the devic in pulm vein
- Wahab technique
- Balloon assisted
- Mitral valve trapping
- Push back
- Multiple methods
Complications – large defects
- Immediate–
– Air embolism – Sheath De-airing
– Rhythm abnormalities
– Groin – Vascular access complications
– Device Embolisation - Early – Pulmonary oedema
- Late
– Aortic root/atrial perforation
Post-procedure management
- Post-procedure management
- Discharged on anti-platelet doses of Aspirin for 6 months
- Can resume normal activities on the next day
- School after 3-5 days
- Follow-up at 3 months, 6 months, year and then SOS